Abstract:
Activated charcoal has long been touted as a miracle substance for detoxification, capable of binding toxins, medications, and even nutrients in the gastrointestinal tract. However, its purported benefits and limitations warrant a critical examination. This thesis delves into the properties and mechanisms of activated charcoal, its interactions with various substances, and its implications for health. By evaluating existing literature and scientific evidence, this study aims to clarify misconceptions surrounding activated charcoal and provide insights into its appropriate use in clinical settings.
Introduction:
Activated charcoal, a highly porous form of carbon with a vast surface area, has been hailed as a panacea for detoxification. Commonly used in emergency medicine to treat poisoning and overdose cases, its purported ability to bind toxins, medications, and even nutrients has led to widespread adoption in alternative health circles. However, the prevailing narrative surrounding activated charcoal’s efficacy and safety warrants closer scrutiny. This thesis seeks to explore the intricacies of activated charcoal’s properties, mechanisms of action, and interactions with various substances, shedding light on its true potential and limitations.

Properties and Mechanisms of Activated Charcoal:
Activated charcoal, derived from natural sources such as wood, coal, or coconut shells, undergoes a process of activation to enhance its adsorption capacity. Through the creation of numerous pores and an extensive surface area, activated charcoal exhibits remarkable adsorptive properties. When ingested, its porous structure attracts and binds substances through physical adsorption, preventing their absorption into the bloodstream.
Activated Charcoal’s Interaction with Toxins and Medications:
One of the most well-established uses of activated charcoal is in the management of poisoning and overdose cases. By adsorbing toxins and drugs within the gastrointestinal tract, activated charcoal can mitigate systemic absorption and facilitate their elimination. However, its efficacy is highly dependent on factors such as the time of ingestion, the nature of the substance, and the patient’s clinical condition. While activated charcoal is considered a cornerstone of toxicology management, its indiscriminate use in non-toxic exposures may pose risks and yield minimal benefits.
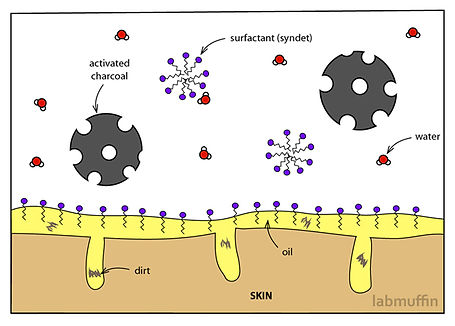
Contrary to popular belief, activated charcoal’s indiscriminate adsorption extends beyond toxins and medications to essential nutrients. Its broad-spectrum binding capacity can interfere with the absorption of vitamins, minerals, and other micronutrients, potentially compromising nutritional status. Consequently, the indiscriminate use of activated charcoal as a detoxification agent may inadvertently exacerbate nutrient deficiencies and undermine overall health.

Dispelling Myths and Misconceptions:
Despite its widespread popularity, activated charcoal is not a universal remedy for detoxification. Misconceptions surrounding its actions, selectivity in binding, and physiological effects abound, perpetuating unsubstantiated claims of its efficacy. It is imperative to debunk myths and foster a nuanced understanding of activated charcoal’s role in detoxification, emphasizing evidence-based practices and clinical guidelines.
Clinical Considerations and Recommendations:
In clinical practice, the judicious use of activated charcoal requires careful consideration of patient-specific factors, including the nature of exposure, coexisting medical conditions, and concomitant therapies. Proper administration and dosing regimens, informed by current evidence and expert consensus, are essential to maximize efficacy and minimize risks. Moreover, healthcare providers should adopt a holistic approach to detoxification, integrating activated charcoal as one component of comprehensive treatment strategies.
Future Directions and Research Needs:
As research in the field of detoxification continues to evolve, there is a need for further investigation into the long-term effects, safety profiles, and optimal utilization of activated charcoal. Novel applications, such as its potential role in gut microbiome modulation or targeted toxin removal, warrant exploration. Additionally, efforts to enhance public awareness and education on detoxification practices should prioritize evidence-based information and promote informed decision-making.
Conclusion:
Activated charcoal holds promise as a therapeutic agent in select clinical scenarios, particularly in the management of acute poisoning and overdose cases. However, its indiscriminate use as a detoxification remedy may yield limited benefits and pose risks to nutritional status and overall health. By dispelling myths and misconceptions, clarifying its mechanisms of action, and providing practical recommendations for clinical practice, this thesis aims to foster a more nuanced understanding of activated charcoal’s role in detoxification and promote evidence-based approaches to patient care.
General References
Wang, Y., Ji, B., & Wu, W. (2018). Activated charcoal-based drug delivery systems for cancer treatment. Colloids and Surfaces B: Biointerfaces, 171, 33-39.
Raveendran, R., Bhuvaneshwar, D., & Praveen Kumar, G. (2016). Activated charcoal: Novel applications in the field of drug delivery. Critical Reviews in Therapeutic Drug Carrier Systems, 33(6), 557-581.
Li, Z., & Zhong, F. (2019). Progress of activated charcoal-based drug delivery systems for cancer therapy. Chinese Journal of Clinical Oncology, 46(14), 785-789.
Jayakumar, S., Murali, M., & Anandharamakrishnan, C. (2019). Activated charcoal-based microencapsulation: A review. Journal of Microencapsulation, 36(8), 717-729.
Duffus, J. H. (2002). “Activated Charcoal” in Environmental Toxicology: Selected Entries from the Encyclopedia of Sustainability Science and Technology. Springer.